- Free Articles
- Shop
- Workshops
- The Dance Educator Series
- L1 – The Fundamentals
- L2 – Pointe Intensive
- L2 – Flexibility Intensive
- L2 – Training Turnout in Tiny Dancers
- L3 – Foot & Ankle Injuries in Dancers – NEW
- L3 – Hip Injuries in Dancers
- L3 – How to Train Extreme Mobility Safely
- Upcoming Workshops
- Workshop FAQ’s
- Workshop Testimonials
- Host Application Form
- Dance Teacher & Health Professional Directory
- Members Areas
- Cart
- My Account
Heel Pain
My daughter gets lots of pain on the back of her heels when she dances and does gymnastics. Sometimes just walking in her school shoes can bring it on. What should she do?
There are several things that may be causing the problem with pain in the back of the ankle, however the two most common are: Retro-Calcaneal Bursitis or Severs Disease.
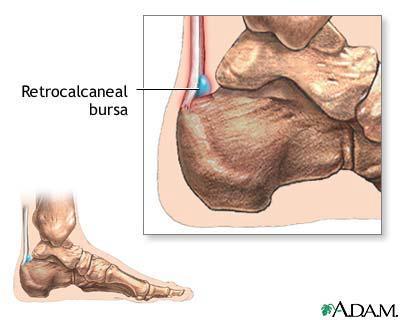
Retro-Calcaneal Bursitis:
At the back of the ankle, the Achilles tendon attaches to the heel bone. To prevent the tendon from rubbing on the bone, there is a small sac of fluid (called a bursa) in between the tendon and the bone. Occasionally, if there is too much pressure over this area, the bursa may become inflamed and the area can get quite painful. This is called “Bursitis” (inflammation of the bursa). The term ‘retro-Calcaneal’ just means “behind the heel bone”.
Common causes of this include:
- Tight calf muscles.
- Shoes that are too small.
- Repetitive trauma.
- An unusual lump on the heel bone (Haglund deformity).
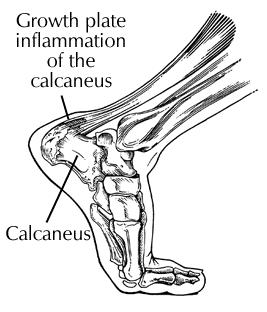
Severs Disease:
Severs Disease is not actually a disease. It is a disorder of local inflammation on the heel that may mimic Achilles Tendonopathy. The Achilles tendon attaches to the site of the major growth plate in the heel bone (Calcaneus) and repetitive pulling at the attachment site during jumping or pointe work may cause irritation, which can be quite painful. This is quite common in young athletes during periods of growth, especially those aged 8 – 12 years. For both of these disorders, the treatment is quite similar. While rest is usually prescribed, it is perhaps more important to learn techniques to reduce symptoms and promote rapid healing.
Treatment may include:
- Training of the intrinsic muscles of the feet to support the arches and reduce the load on the big calf muscles.
- Taping techniques to reduce the load that is put on the Achilles attachment point.
- Soft tissue massage to release tight calves.
- Padding on either side of the irritated area to reduce the pressure (padding over the area may increase the pressure and further aggravate symptoms.
- Pelvic stability exercises.
- Gluteal activation exercises and re-education of walking.
- Gentle stretching of the calves.
- Restricted hours of dance and avoidance of certain activities within classes.
- Cessation of pointe work.
- Gel heel cups in street shoes.
- Soft “orthotic” devices in street and sports shoes.
Return to full classes should be taken gradually when symptoms are settled, and care should be taken if there is a second growth spurt. Always be guided by your doctor or physical therapist for the most appropriate time. A good way to monitor growth rate is to measure your daughter’s height every two weeks against the side of a door (remember to take off her shoes!). This will give you a guide as to when she must take care of the number of hours of dance she is doing, especially involving jumping, to prevent the likely hood of the severs disease reoccurring or the development of other pains related to bony growth.
Injury & Foot Resources
If you are looking to delve deeper into this topic, check out the following programs:
- Will I Ever Dance Again: The “Will I Ever Dance Again?” program is perfect if you are unable to train at full capacity, whether this is due to a foot injury, surgery, an accident or illness outside of the studio. It helps you build back to full capacity gradually, while maintaining strength, flexibility and control in the rest of the body.
- Level One Dance Teacher and Therapist Training: This unique course covers a multitude of assessment and treatment techniques to individualise a dancer's training. With special focuses on Postural Control, Core Stability, Flexibility, Basic Classical Technique, The Dancers Hip, Allegro, Spinal Mobility and Arabesques, it is suitable for anyone working closely with dancers.